Thank you for your input Thomas. I was offered treatment last january and I kept putting it off. I was offered Tenofovir because I’m still childbearing age. I started it last night and will have another blood test in 4 weeks to see the effect of it. I hope I made the right decision ![]()
Sounds good, @dianawhite! Hope it all goes well, please keep the community up to date on how you go!
TT
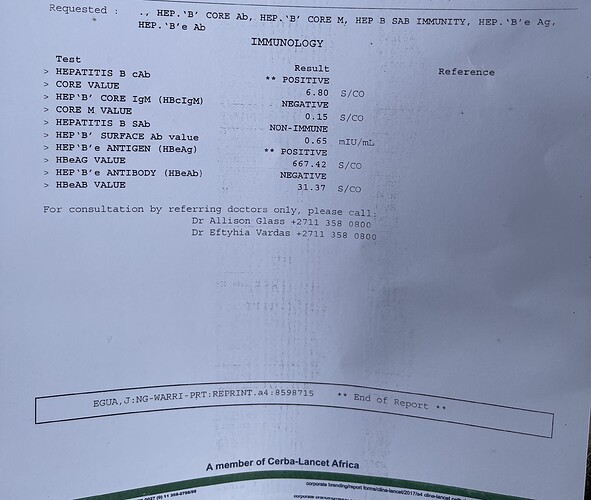
Hi experts, this is my hepatitis b profile test. I have these questions;
based on this results can I start taking tenofovir.? Because of hbeag.
My lft are ok .
Just worried because Hbeag is positive.
Do you start to take anti virals when you have high viral load or when it’s starts affecting the liver? I’m currently 7 months pregnant.
Dear @anni2,
Thanks for your question and welcome to the forum. Under most guidelines, you would need to have a HBV DNA test to determine if you should start antivirals: for pregnant women, treatment should be started if HBV DNA levels are above 200,000 IU/mL (AASLD guidelines).
Thomas
Can a pregnant woman with high or low virals who’s hbeag positive transmit to baby in the womb or the transmission happens during birth
when vaccines were not given on time?
I don’t want my baby to be positive ![]()
I want to take all precautions!
Hi @Anni2,
One of the experts will field this question as my knowledge is limited in this area. However, here are a couple of threads that I found on the subject that you could read up on until an expert can respond. I hope this helps.
-Paul
https://www.hepbcommunity.org/t/hepb-transmission-from-mother-to-child-when-low-viral-load/1311/2
https://www.hepbcommunity.org/t/having-children-and-hepatitis-b/166/2
Dear @Anni2,
Transmission generally does not occur in the womb, but occurs during the birth, which is good because it allows some opportunity for the doctors to treat you and the new-born to prevent infection. There are several interventions that can be used including:
- Treating you with antivirals close to the birth, so that you have lower viral load and therefore less risk of transmitting.
- Providing the newborn with antibodies against the virus, which would stop the virus from infecting the liver and spreading.
- Immediate vaccination of the newborn straight after birth so that they make their own antibodies to fight off any potential transmission.
Some or all of these can be used, depending on your situation. You should discuss this with your doctor/midwife/obstetrician to plan.
There are many Hepatitis B positive mothers on this forum who have successfully prevented infecting their children (see Having children and Hepatitis B).
Hope this helps a bit,
Thomas
Thank you for your time.I really appreciate.
Also ,is it only people with high viral load that ends up having liver issues or pains almost every day?
Currently on anti virals but still having this liver heat and pains .scan and lft says all is normal.
Does anti virals help the liver to heal .
I was infected with this virus just last year but started taking anti virals because of positive hbeag value of 600+ and also fear of transmission to baby.
Dear @Anni2,
The liver issues/pains are a complex interaction between the virus, your liver and your immune system. It isn’t automatically given that if you have high viral load, you have pain.
The antivirals will help your liver recover from any injury caused by the virus. If you are still feeling pain in the area, it may be possible that it is being cause by other issues that you should talk to your doctor about.
Hope this helps,
Thomas
Thanks for your replys. Lastly, I would like to know if TDF has no birth defects or has effects on my baby’s growth as I’m taking it.wouldn’t want my child to have any issues.
Dear @Anni2,
As mentioned in other threads, TDF is the recommended treatment during pregnancy and is not linked to birth defects.
Hope this helps,
Thomas
Hi everyone, this is David, I am new here and am greatly educated by the valuable discussions and experts in this forum. Thank you for everything you did to educate and help!
I am Male, 40yrs, Asian, infected with the virus from the birth (my mom has hbv infection).
ALT is normal and stable since the past 12years when the regular check was started, with the E antigen keeping non-reactive over the years (I remembered the E antigen was reactive about 20 years ago when i did the first blood check, knowing that I carry the virus.)
Unfortunately the HBV DNA was not always tested each time, but with viral load log of 2 for these being tested in the past years.
In this March, the hbv dna raised up to log of 4, ALT and ultrasound keeps normal.
I personally prefer to take the antiviral drug considering my age and family history of the disease. However, one of the local hepatologist would like to keep monitoring the condition, his opinion is that I have normal ALT and not high viral load. Also, he believes that for E antigen negative patient, the antiviral medication may not bring the viral load down to very low or undetectable range.
Could the expert provide some inputs for my case? Thanks very much.
Hi can the expert comment on this? Thanks for the help
Dear @DZ6,
Thanks for sharing your story and sorry you’re feeling stress over this. The antivirals will generally still work in HBeAg-negative phase to lower HBV DNA levels that you are showing.
Can I ask what is the family history of Hep B? Any instances of liver cancer?
My personal opinion is that one should start treatment sooner rather than later, but this is definitely something that you’ll need to discuss with your health provider about what’s right for your context.
Hope this helps,
Thomas
Thanks very much Thomas for your kind attention. Correct, my Mom died of HCC.
Today I visited my hepatologist and discussed the family history, who still did not recommend the antiviral drug for my case; he believes i would gain less especially the fibroscan result of F0-F1. He expects me to take regular check and visit him every six months.
He did mention that he can treat me if I strongly wish so, and highlight the side effect of TAF would be mainly weight gain. He said, although the family HCC may scares me, he believes the major cause of such family tragedy is due to lack of health check and timely treatment as needed (he believes direct HCC by hep B virus is extremely rare).
I consulted with him on the new involvement of treatment expansion in US and China, he replied he keeps abreast very well of these progress and also very familiar with the experts who developed the guideline. He politely educated me that the way he treats me is supported by his decades of clinical experience with thousands of his patients and their outcome. His fellow mentioned to me that, part of the reason why the treatment criteria was expanded is because lack of regular check and monitoring for many people who are able to access.
I was somehow convinced as the place I visited represent the best specialist in the country I live. So I fully respect the doctor’s medical opinion and leave the treatment request in the next regular check with him after thorough consideration. At the same time, it seems hep B is a complicated disease we actually don’t know exactly what is happening inside the body even there is mature guidelines can be used.
Therefore, would you pls help me input further so that I could make mature decisions?
Thank you very much.
David
Is weight gain really a side effect of TAF?
Or is it rather TDF (the “older” tenofovir) has some lipid-inhibiting off-target effect, which TAF doesn’t have (and, as a result, people switching from TDF to TAF might experience some weight gain)?
I’m personally 3rd year on TAF, my weight is stable, BMI within norm, I eat what is considered healthily (vegetarian/pescatarian diet) with moderate amount of exercise.
Dear @DZ6,
According to the EASL guidelines:
Patients with HBeAg-positive or HBeAg-negative chronic HBV infection and family history of HCC or cirrhosis and extrahepatic manifestations can be treated even if typical treatment indications are not fulfilled (Evidence level III, grade of recommendation 2).
So you are within your rights to consider therapy given your situation. However, this is of course a personal decision and needs to be made with your own context in mind.
On the research side, there is more and more evidence that there are cancer-associated changes occurring in the liver, even before it is observable clinically (e.g. liver inflammation has been reported even with normal ALTs; there is HBV DNA integration decades before cancer, etc.). It has not been directly shown that these will lead to cancer down the road (which is why such early treatment is not a recommendation), but there is also lack of evidence against it too.
For my own decision, I have thought about which side I want to err on: treatment before it is necessary to prevent chances of ill-effects, or waiting too late and not catching the liver damage.
Hope this helps frame the current understanding in a way where you can make an informed decision.
Thomas
Hi DZ6,
Welcome to the forum and thanks for sharing your story and experience with us all. I am of the same opinion as Thomas, that when it comes to treatment it should be started early rather than later. And also if a patient want to start treatment they should be able to do as well. This opinion seems to go contrary to the treatment guidelines. What I will suggest is to continue to have an open and honest conversation with your provider regarding this. Let him/her be aware of your worry or concern and how you really feel about treatment. I did not start treatment immediately, rather it was almost 2 years after my diagnosis before a treatment was recommended. This can vary between providers. I think the important point is as long as the provider is talking to you, explaining things so you can understand and be able to ask questions along the way; and you are open to the provider, things should be alright. Keep this conversation going with your provider so you can get frequent updates on where things stand and whether anything has changed. keep your appointments so the monitoring can continue, very important.
Best, Bansah1.
Hi @many723,
Reminder that I am not an expert in the field or a medical professional.
-
I think the short answer is that CHB is pretty much the same regardless if it is acquired at birth, as a child or as an adult. The experts may have a more elaborate response to this. As to your upper right quadrant pain, this is a perplexing issue as doctors will tell us that the liver doesn’t feel pain but yet, so many of the affected community experiences this pain. There are so many posts in these forums about this particular pain and other pain that have yet to be associated directly to HBV, CHB or antivirals.
-
I do not know the answer to this so we’ll have to wait for the experts to respond, but here is the definition from The Hep B Foundation: IgM anti-HBc: A subclass of the hepatitis B core antibody (HBcAb or anti-HBc). Positivity indicates recent infection with HBV (less than 6 months). Its presence indicates acute infection.
-
I think it depends on how severe your diagnosis is, but the best beginning rule of thumb is, all things in moderation. However, you want to eliminate or keep anything toxic to a minimum like smoking, drinking, etc. When it comes to going out to eat, when done in moderation, you can look for healthier alternatives. Less fried or processed foods, less salt, less fat, more protein and more fiber. For example, they make some pretty good tasting entrée salads nowadays. Maybe opt for an Asian chopped chicked salad instead of the fried chicken sandwich. I know it can be so tempting but you can find better for you, but still tasty alternatives when you go out.
Lastly, I know it’s easier said than done but don’t stress yourself out so much about your upcoming ultrasound. Don’t worry about HCC and cirrhosis if/until you get to that road. Stress only makes your liver work harder. Again, easier said than done. Be sure to update us once you have the results of your ultrasound and until then do your best to distract yourself from it and not focus on it.
-Paul
Dear @many723,
That’s a great question and I think the real answer is we don’t know. There is some evidence that maybe it is different: there are particular genotypes in areas of the world where adult or horizontal transmission is the more common route (e.g., Genotype A in North America and Western Europe). This appears to be more responsive to interferon and results in more HBsAg-loss if there is cessation of long-term nuc therapy. Whether this is due to the genotype itself or the mode of acquisition is not very clear.
As mentioned by other users, anti-HBc IgM is seen when a person has been exposed to the virus for the first time in the last few months. The result of this exposure (whether it becomes chronic, or if it is cleared and is an acute infection) depends on multiple factors, including age as you’ve just mentioned.
We have a few threads about this: Lifestyle changes, nutrition, and supplements for hep b, Food, Activity, and habits alternatives guid; and Vices - alcohol marijuana etc.
Hope these help,
Thomas