Yes, these numbers can naturally go up and down.
Hi Docs and all member,
I had HBV since 2006. I start taking TAF from 2016 until now. Recently I have a few concern with my health since I feel my skin got a little bit yellowish than normal. I got a HBV and Liver Function Test on early September. everything is normal except I got a little bit of Ferritin (iron) elevated.
Here is my blood test result
Ferritin = 732 ng/ml
Bilirubin Total = 1.1 mg/dL
Bilirubin Direct = 0.3 mg/dL
ASAT = 18 UI/L
ALAT = 17 UI/L
Alkaline Phosphatase = 66 UI/L
GGT = 30 UI/L
Amylase = 64 UI/L
Albumine = 45g/l
AFP = 2.6
Fibroscan (echosen) = 3.0 kPa
Antigen Hbs (quantitative) = 1426 UI/mL
HBV Viral is undetected
With these result my local doctor said I am normal. however, I feel my skin color is a little bit yellow than normal during the last few months. shall there be any missing test? shall there be any recommend regarding my skin color change?
thank
My husband was diagnosed with HepB in September when he went to ER for abdominal pain. At that time his Alk Phos was 139 Int._Unit/L (High), ALT 776 Int._Unit/L (High), AST 558 Int._Unit/L (High), and Bili Total 0.8 mg/dL. Those were from September 26th.
Since then they said this was no big deal, your body will clear this on it’s own and we will just do routine blood tests to monitor it. He has continued to decline and now has jaundice.
Oct 19th - ALT 795, AST 710, Bili Total 2.8
Oct. 26th - ALT 813, AST 733, Bili Total 7.5
Oct 28th - ALT 757, AST 665, Bili Total 10.8
Oct 29th - ALT 756, AST 679, Bili Total 10.2
No one will explain what this means. They are only giving him morphine for pain? He has had 2 ultra sounds that came back normal and “unremarkable”. So signs of tumors, scarring, or abnormalities in size or shape?
His HepB Core Ab,Igm was reactive as was his HepB SurfaceAg. His SMA was positive and his AMT was 1:80.
Dear senhour,
Based on the test results, your HBV infection si very well controlled. There is no evidence of liver dysfunction. Your total bilirubin is VERY slightly above the normal range but this does not indicate something is wrong. Your bilirubin would have to be much higher to affect the color of your skin.
Any dietary changes? Are you outside more often then previously?
Dear SamanthaMech,
Your husband has acute hepatitis B. Based on the results you have provided, your husband should be put antiviral therapy (entecavir or tenofovir disproxil fumarate) given the progressive and large increases in bilirubin. This is a sign that his liver is not functioning correctly. He may feel increased itching as a result of this elevated bilirubin.
Regardless of “unremarkable” ultrasound findings, there is a clear biochemical decompensation of your husbands’ liver function (as evidenced by his jaundice, which is caused by the very large increases in his bilirubin) which should not be allowed to persist if it does not start to immediately self resolve.
The current attending physician(s) is likely be operating under the assumption that his infection is acute (HBcAg IgM positive) and will resolve (as it does in ~80% of patients). However, the severe nature of the biochemical decompensation in your husband (bilirubin elevations) demands real supportive therapy to normalize liver function (antiviral therapy).
Best of luck.
Thank you SO much for the information. I have gotten no where trying to ask questions of these doctors here. No one will bother explaining anything and any time I ask questions they basically don’t answer and just say I am “ill informed”. I have been reading so much information here and the Drs at the hospital just make me feel like I’m crazy? After 3 days of my husband sitting in an ER getting pain meds and NOTHING else, they have finally moved him to a real room and admitted him this morning. Since he was in the ER, they would not allow me to stay with him, so I am heading to the hospital to see what they are doing and why they finally admitted him after 3 days.
Again, thank you so much!
Hi SamanthaMech,
I am sorry to hear you are getting such a poor level of communication and consideration from the physicians. This is of course ABSOLUTELY unacceptable and unprofessional.
The medical facts are pretty obvious:
- Your husband has acute HBV.
- Your husbands’ liver function is decompensating. While the body can tolerate reduced liver function for sometime without lasting effects, the clear progression of reduced liver function in this patient should be cause for alarm and should be prevented if possible. Pain management will do nothing to treat this underlying issue.
- The use of NUC therapy is indicated to control the progression of liver disease in patients with chronic HBV. Current treatment guidelines indicate that waiting for acute HBV infection to self-resolve without therapy is only acceptable if the underlying hepatitis is not fulminant (which his bilirubin results indicate his hepatitis is).
The United States guidelines from AASLD are very clear on this point see page 1579 (section 6E) in https://aasldpubs.onlinelibrary.wiley.com/doi/epdf/10.1002/hep.29800.
The European guidelines from EASL are also equally clear see page 387 in https://www.journal-of-hepatology.eu/action/showPdf?pii=S0168-8278(17)30185-X.
Good luck!
They refuse to administer antivirals of any kind. They are not a transplant hospital and because of that they say they cannot administer the meds. I have asked the attending Dr to contact another hospital that has a hepatologist and see if they are willing to administer the medication. He said he will call, but if they do agree and anything goes wrong, they too will have to try transferring him to a transplant hospital in Cleveland Ohio for my husband to receive the proper care or a transplant if needed?
They did finally admit him to this hospital and put him back on IV fluids. They also gave him Acetylcyitene to rid his liver of any Tylenol products. This just caused massive puking for an hour? 
I am currently waiting to hear if the other hospital near me is capable of administering the meds and/or for Cleveland clinic to have an open bed to treat him.
Again, I appreciate and thank you immensely for the information you have provided. I atleast have some hope that my husband could recover with out a transplant.
Dear SamanthaMech,
To be frank none of the statements made by the doctors make any sense. TDF is the recommended and the preferred NUC for controlling fulminant hepaitis during acute HBV as is stated in the guidlines.
Atleast he is admitted with supportive IV.
I hope this turns out ok for your husband.
Dear @availlant
Thank you so much for explanation and that it is not big concern. Anyway I have a few more concerns.
I am living in Cambodia, Southeast Asian Nation. I go out to work to work and exposed to sun light daily.
I think I don’t have any majore change in diet except I start to increase my vegetable consumption. Especially leafy green and cruciferous vegetables
1 - is there any indication that bilirubin will continue to increase?
2 - does my skin pigmentation could be related to ferritin level ?
3- how can I do to lower down bilirubin?
Thank
HI Senhour,
I don’t see any reason from the data you provided to expect that your bilirubin is troubling or will change over time but you should be followed on antiviral therapy every 6 months. However, elevated ferritin levels can result in a change in skin pigmentation. There are many possible reasons for elevated ferritin these should be investigated by your doctor.
Best regards,
Hi @availlant
Thank again for more explanation. Yes my doctor told me to go back and check everything again in 6 months or less if I notice any major change to my body.
I will surely follow strict diet and continue on my TAF treatment.
No alcohol
No junk food
Less sugar
Less high fat food
More vegetables
Do regular exercise
Try to reduce stress
And have enough sleep
I will surely posting my updated blood test result in the next few months.
Thank
Hi @availlant
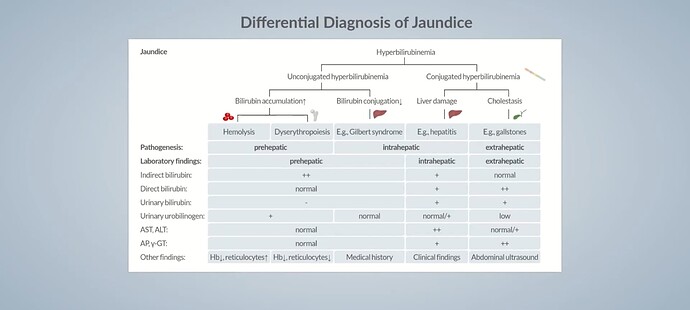
I think I found the answer to my condition right now. Actually, jaundice is classified in three type Pre-Hepatic, intra-hepatic, and Post-Hepatic.
Based my felling of yellow in my skin ( I personally notice myself through in house under LED light with different light color variations (different color tone), outdoor under bright sunlight or cloudy sky.) I can conclude that my skin is a bit yellower than my normal skin.
According to this Jaundice Lab analysis video Jaundice: Differential Diagnosis - YouTube And my previous blood test result I personally think I got Pre-Hepatic jaundice
The indicators can be taken from previous blood test result are
Bilirubin Total = 1.1 mg/dL
Bilirubin Direct = 0.3 mg/dL
ASAT = 18 UI/L
ALAT = 17 UI/L
Alkaline Phosphatase = 66 UI/L
GGT = 30 UI/L
Amylase = 64 UI/L
Albumine = 45g/l
Red Blood Cell is a little bit lower than normal
According to this video to conclude Pre-Hepatic Jaundice are
Slight elevated Bilirubin
Normal Liver Function Test
Lower Red Blood Cell
If you have more explanation please.
Dear senhour,
The upper limit of normal for total bilirubin is 1 mg/mL in most countries. Your reading of 1.1mg/mL is not really an increase which would be consistent with yellowing of the skin (or prehepatic jaundice). Jaundice is associated much higher levels of bilirubin than your tests indicate and will also be accompanied by a yellowing of the whites of your eyes (sometimes appearing brownish).
Again the elevated ferritin is the more likely culprit here but additional blood work is needed.
Unless this your skin condition changes and or your eyes become discoloured, I would relax on this issue but be sure to discuss it with your physician at your next visit.
Hope this helps.
Dear @availlant
Thank again for your explanation. I can’t wait to do the next blood test. I probably will go to do sonner than normal appointment which is 6 months.
Hope everything gonna be okay.
Thank again for your responsive reply.
Hello everyone! I posted a few months back about my moms hep b tests, and I’m back with some updates and questions. My mom is 70 years old for context.
The results were as follows:
Hbsag: negative
Hbcore: positive
Hbsab: negative
Alt: 11
AST: 25
AFP: 2.6 ng/mL
After we got these results, her doctor ordered hep b vaccination because we initially thought it was a false positive hbcore, and she’s had 2 out of 3 shots. We just got results back from her hbv dna, and it’s as follows:
Hep b dna: 135 IU/mL
Hep b viral load: 2.13 log
So I have two questions with her new results (the dna results),
-
Could the dna results be a false positive due to recent hep b vaccination? I’m grasping at straws so I’m sorry if this is a silly question.
-
Is it a good sign that her hbsag is negative, even though her dna is detectable?
Thank you so much for your time! I’m a nervous wreck when it comes to my mom’s health, and the doctor released her dna test results with no comments so I’m spiraling with anxiety about what it means.
Hi @availlant
I may want to include the talk about Vitamin D and Liver Disease association.
Recently about 1 months early I started to notice my skin look pale ( I thought I got Jaundice) but my local doctor and Doctors in this forum explanation it is not Jaundice based on my result.
However I am not quite calm with the situation I try to understand more about related condition. I found one video in YouTube talking about Anemia of Chronic Disease which also link to Liver Disease. I look back on blood test result. I found something could be related.
My result
- Red Blood Count ( RCBs) = 4.1 T/L
- Hemoglobin = 13.4 g/dL
- hematocrit = 38.6 %
- HCV = 95 fI
- Vitamin D = 22.14 ng/mL
I could see that I Amy probably fall into this category. Moreover, I found research about Vitamin D and Hepatitis B association say that Vitamin D defeciency may increase risk of cirrhosis and liver cancer.
Please any suggestions or recommend?
The research
The video about Anemia of Chronic Disease
Dear Lily_Lee,
Your mom has HBV infection but not hepatitis. She has what we call chronic “inactive” HBV where the the replication of virus in her liver is very weak so as to not cause liver disease. All HBV vaccines only contain HBsAg as the antigen so the HBV DNA result cannot be caused by the vaccine doses she has already had. Which vaccine is she receiving?
Her negative HBsAg test (with positive HBV DNA) is unusual but also a good sign. If possible, she should be followed every 6 months for HBV DNA evaluation. There is no point of introducing antiviral medication at this point.
Best regards,
Dear senhour,
Your hematology results are unremarkable (essentially normal). However your vitamin D is low.
As you have discovered, are some studies linking vitamin D deficiency with HBV progression. In your case it cannot hurt to take a vitamin D supplement.
Best regards,
Thank you very much for the clarification and response! Her doctor started her on Engerix-B after her HBsAg-, HBcAb+, HBsAb- result, but that was before we got the results for the DNA testing. She’s had 2 doses so far.
Now I wonder if it’s pointless to continue the vaccination series since we have confirmed that she has the DNA, but she only has 1 dose left so I suppose it can’t hurt!