Hello, my name is Xinrong Zhang, a posdoc from Dr. Mindie Nguyen’s Lab, School of Medicine, Stanford University. I am studying the linkage between HBV and altered metabolic dysfunction recently.
Chronic hepatitis B (CHB) is one of the leading causes of cirrhosis and hepatocellular carcinoma (HCC), affecting more than 296 million individuals worldwide and resulting in an estimated 887,000 deaths annually. The increasing prevalence of metabolic syndrome, comprising diabetes mellitus (DM), hypertension, obesity, and dyslipidemia, has become one of the most challenging public health problems around the globe. Its associated metabolic dysfunction-associated steatotic liver disease (MASLD) has also become the fastest rising cause of chronic liver disease. Both metabolic syndrome and MASLD are associated with increased risk of liver complications such as HCC and cirrhosis, as well as non-liver complications such as cardiovascular disease (CVD), chronic kidney disease (CKD) and extrahepatic cancers. Moreover, with the obesity epidemic, metabolic diseases and CHB are increasingly seen together and may alter the natural history of CHB with potential synergistic interaction and association with future adverse clinical outcomes. However, comprehensive and detailed natural history data characterizing the relationship between the individual as well as combination of metabolic risk factors (MET) on CHB disease progression and adverse liver and non-liver complications are still sparse.
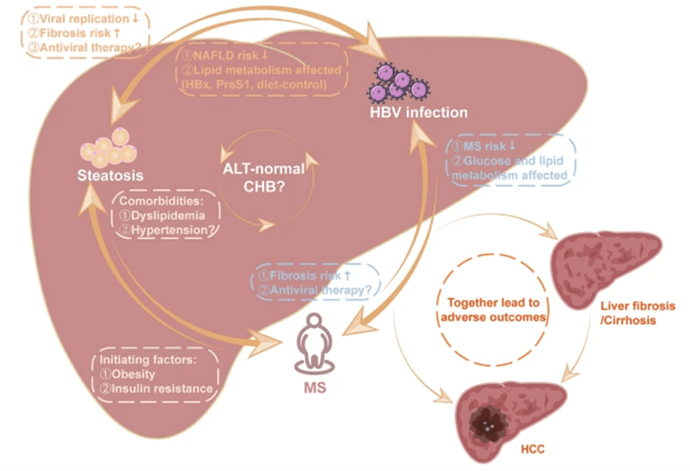
Figure 1. The relationships of metabolic syndrome, hepatic steatosis, and HBV infection (cited from Yuting Diao et al. Infect Dis Ther. 2023 Jan;12(1):53-66.[https:/pubmed.ncbi.nlm.nih.gov/36441483/])
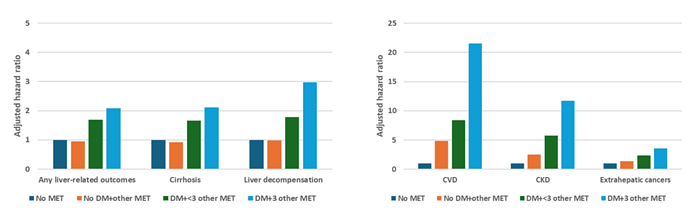
As the global CHB patient population ages, more metabolic comorbidities in CHB patients should be expected, monitored, and managed appropriately. Therefore, we aimed to investigate the association and synergistic effects of MET on the risk of adverse liver and non-liver outcomes including CVD, CKD and extrahepatic cancers in patients with CHB. We conducted a retrospective cohort study of 39,882 adult CHB patients derived from a database of privately insured US people between 2007 and 2021. We used propensity score matching to balance the baseline differences of CHB patients with MET and without any MET. We found that a higher burden of MET, particularly DM, was incrementally associated with greater risk for liver and non-liver complications. Additionally, we found that not all metabolic components were equivalent with DM which was found to be the strongest risk factor for adverse liver outcomes. There was no significant difference between CHB patients without any MET and those with MET but without DM in our study.
Figure 2. Association between the burden of MET and adverse outcomes in patients with CHB
Together, our data may highlight the importance of a multidisciplinary approach to the clinical management of patients with CHB and metabolic diseases especially those with DM, and to inform future cost-effective screening and prevention of liver and non-liver morbidity programs with more precise risk stratification estimates.
Thank you for reading and looking forward to your questions!