Context:
- 55F. Chronic HBV since 1994. Not on medication. See a GI every 6 months.
- In Apr 2022, ALT spiked to 64, and viral load E+05. Ultrasound OK. Fibroscan OK. ALT later went down to 40ish. Viral load E+04. I have stopped taking multivitamin since the spike.
- One week ago (mid Nov 2024), ALT 53, AST 39. Ultrasound OK. Not sure what caused the spikes. I maintain a pretty healthy lifestyle because I have been recovering from chronic MDD and GAD. I don’t have any other major medical conditions.
- I will have another lab in 3 months, see a hematologist in 6 months for consultation, and then I will begin treatment.
Questions:
- I had HAV vaccination in the US in 1999. My antibody was still good in 2018 when my family doctor last looked into it. Do I need to get another shot?
- In the past year, the only change in my diet was that I add Walmart’s organic wild blueberries in my oatmeal with milk in the morning. Can I eat blueberries?
- I use Olay face cream and Aveeno body lotion. Can I use any of these?
Thank you and happy holidays to everyone.
Hi @babytobeast,
Welcome to the community. Thanks for sharing your experience and status with us all. For your first question, HAV vaccines have similar effectiveness as the one for hepatitis B. Most people build long lasting protection against this virus. Only a small sample of people loses that protection over time. I doubt you are one of those individuals so I don’t think you need one especially when your 2018 results showed you were still good with your antibody.
For the second and third questions, there are no diet or skin care product restrictions for HBV patients. You can eat anything you want, just avoid too much alcohol, fried foods and smoking. Remember, the key is everything in moderation. Blueberries are actually a good food source of antioxidants and other nutrients. You can use any skin cream or body lotion that works for you, as long as your skin does not react negatively to it. It should not affect your HBV in any way. Best, Bansah1
Dear @babytobeast,
Thanks for your questions!
- I’m not sure if you are at greater risk of being exposed to HAV in your work or because of where you live. If you are, the best course of action may be to check your antibody levels again and see if you need a booster. As mentioned by @Bansah1, antibody levels can be maintained for many years.
- There is generally no restrictions in particular foods, and blueberries sound great (one of my favourite berries).
- I have not heard of any sort of face cream or topical lotions being harmful (whether you have hep B or not).
Hope this helps and happy holidays to you too!
Cheers,
Thomas
typo. will see a *hepatologist in 6 months for consultation.
1 Like
Thank you @ThomasTu @Bansah1
More test results:
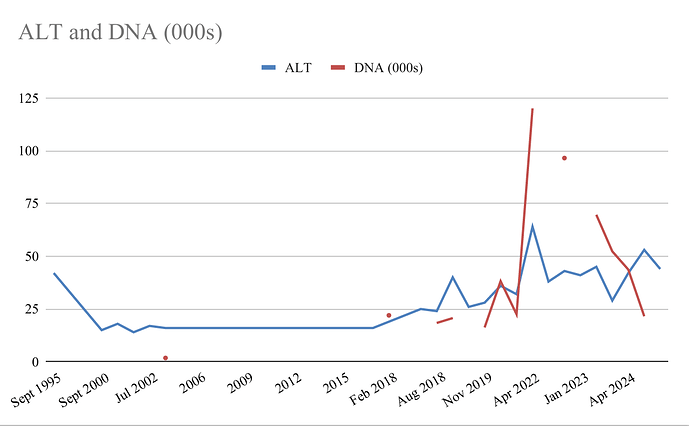
Jun 2021, DNA(IU/ml) 2.25E+4, ALT 32
Apr 2022, 1.20E+5, 64
Jul 2022, n/a, 38
Oct 2022, 9.65E+4, 43
Jan 2023, n/a, 41
Apr 2023, 6.96E+4, 45
Oct 2023, 5.23E+4, 29
Apr 2024, 4.37E+4, 42
Nov 2024, 2.16E+4, 53
Follow-up questions:
- Viral load has declined consistently after the spike in Apr 2022 while ALT has been down and up. Does this mean my 50-year-old immune system finally “wises up”, recognizes mutated viruses, and has been fighting the viruses as well as host liver cells?
- Why did ALT go back up in the past 12 months while viral load continues declining? I suppose this is not a good thing, isn’t it?
- Anti-HBs has been less than 5 mIU/ml since we began to track in 2018. Is this caused by virus mutation as well? My HBeAg has been negative for decades.
Thank you very much.
Hi @babytobeast,
It’s normal for the ALT and AST to fluctuate from time to time. It’s a concern if it remains high over multiple tests for some period.
Sometimes, the virus remains dormant and doesn’t cause any issue known as inactive phase. In this phase the virus stays low for sometime. Unless something happens to trigger a flare-up which then can cause an increase in viral load. I hope this is helpful. Bansah1
Thanks @Bansah1
In my case, the trigger in 2022 was probably a combination of 1) menopause, 2) switching from centrum to jamieson to one-a-day women, 3) stressful life event, and 4) not enough sleep for a few months.
I am trying to understand why my immune system suddenly got into a fight with the viruses after they seemed to have got along for decades. Is it due to weaken immune system that cannot suppress virus replication, OR due to the adaptive part of the immune system that finally recognizes mutated viruses?
It’s hard to say. Our immune system is very complex and not easy to explain why it’s fighting your virus now but not in the past or vice versa. All the issues you mentioned are all key but the one’s that are more likely to affect your immune system are stress and lack of sleep. Those two can put your immune system out of shape. Let’s hope things have improved.
There are no straightforward answers to your questions because we are dealing with two complex issues (HBV and immune system). Best, Bansah1
Dear @babytobeast,
You’re correct. In general, liver inflammation (ALT increase) is associated with reduction in viral load, as it represents the immune response trying to clear infected liver cells.
The anti-HBs is expected to be low if you have detectable virus load. This is because the HBsAg is expressed at very high levels. It is not due specifically to virus mutation.
Thomas
Thank you @ThomasTu @Bansah1
I just got a call from hospital. I will see the hepatologist for treatment consultation on Xmas eve! Got to be Santa watching over me 
I have the following issues to ask the hepatologist:
- Treatment options. My brother was switched from TDF to ETV when he was 45 and had treatments for early stage liver cancer. I am concerned what TDF might do to my 55-yr-old kidneys and bones. I’d try Vemlidy if there are ways to pay for it. If I have to take generic, I’d take ETV. Thoughts?
- Does switching between ETV and TAF cause any side effects or drug resistance?
- When do I need to get tested for qHBsAg?
- My brother’s AFP was normal even when he had liver cancer. So he got tested for DCP. Do I need to get tested for DCP?
- During treatment, do I need to baseline and track the following 5 issues? 1) Lactic acid levels; 2) Bone density; 3) Renal tubular dysfunction; 4) Cholesterol; 5) Diabetes. My first-degree relatives have both hepatitis b and type 2 diabetes.
What else should I ask the hepatologist? Thank you very much.
Hi @babytobeast,
Yes, you can switch antivirals with guidance from your doctor. For example, I was on ETV then switched to TDF at some point because my results were fluctuating after many years on ETV. I had to switch to Vemlidy after a number of years being on TDF because there was some evidence of early kidney problems. I recently went back to ETV because of increased cholesterol and I was not prepared to begin taking statins with the understanding that if my numbers begin to rise I will go back on Vemlidy. I did this in consultation with my hepatologist and after multiple conversations we decided to do the switch and continue monitoring. Don’t switch by yourself, please. All these antivirals are effective, except that some patients tolerate one more than the others. They are all great otherwise.
Because you have a family history of liver cancer and diabetes, I will suggest that you bring all these questions to your doctor, have a dialogue, develop a plan for your care, and continue to be monitored. That will be my advice here. Having this conversation with your doctor will help address all your questions regarding what to do (such as tests) or keep an eye on etc. I hope this is helpful. Bansah1
1 Like
That’s great that you have got a consult soon. Also great that you are making a list of your questions, @babytobeast. It is indeed one of the suggestions that we brought up in another thread, which may be useful to you: Tips on making the most of your consults
TT
How did you manage it by far so well ? What is your lifestyle??
Thanks @ThomasTu @Bansah1
Updates:
- So I spoke with the hepatologist. Initial response is that it is up to me - I can continue to monitor another year or begin treatment now. This is mainly because 1) my fibroscan is 5.7kpa (F0) not fasting, 2) ultrasound normal, 3) AFP normal. My risk factors are 10E+04, ALT 40ish, age 55. My brother had HCC however he lives in an endemic country with a very different lifestyle. I will see the doc again next year to make a decision.
p.s. qHBsAg is 1226 mIU/ml. Not sure if this is good or bad.
Question:
- Do I need to provide the doc my medical history before 2018? The healthcare systems here has my labs, etc. since 2018. I had lived in other countries so it will be a pain to gather all the reports decades ago. I do keep a spreadsheet so a 30-year history is as below. I was first diagnosed in 1993 when I was 24, with active HBV (HBeAg+), ALT 42. My HBeAg became negative in 1999 when it was tested again. ALT 24. Platelet count ~300 E9/L. Platelet count now is 180ish (low normal). I had been inactive until 2018/19.
Thank you very much and happy new year to everyone.
Hi @babytobeast,
Thanks for the update. If I were in your shoes, I will start treatment now and not wait for next year if this is possible to me. Your family members history of HCC puts you at risk despite the environmental exposures and lifestyle they may have. But you need to make that decision and I am glad your doctor gave you that respect and opportunity to decide.
As per sharing medical records, I doubt it will be necessary unless there is something that had happened in the past that has changed over the years. The ALT and HBV DNA graph or curve is helpful in creating a great picture of your journey with HBV. If the doctors asks for these records, then yes you can try and get them, if not then I will suggest you don’t have to worry too much about it. Best, Bansah1.
eat right, exercise, sleep well, manage stress.
Thanks @Bansah1
I didn’t get the impression that the doc was just being polite. He seems to be one of those docs who do not believe in treating everybody ASAP. AASLD 2018 has not been updated despite drugs today have fewer side effects and less drug resistance. So I wonder what the arguments would be.
Sure, there are doctors like that which I think it’s good. Because, it will be troubling to put someone on treatment and due to access issues they can’t successfully adhere to their care plan which can lead to more trouble.
WHO has a new treatment guidelines. It’s always been accepted to treat people with family history of HCC. If possible have a discussion with your doctor about the pros and cons of all available medications. Best, Bansah1
2 Likes
Dear @babytobeast,
These are good results with the fibroscan as your liver appears healthy at F0. Indeed a family history of HCC (regardless of differences in lifestyle) does make the case for treatment stronger - as mentioned by @Bansah1 this is an indication for treatment under current guidelines.
Regarding your results from before, it may be sufficient to provide this graph (great self-advocacy!). It does show that your ALTs used to be lower suggesting that there is some degree of liver inflammation despite your ALTs being within “normal” limits. Being on treatment will minimise this inflammation.
Hope this helps,
Thomas
2 Likes